Overview
With funding from USAID’s Center of Excellence in Democracy, Human Rights, and Governance (DRG), CIRGH assists HEARD in its efforts to strengthen the evidence base and accelerate data liberation and evidence use related to community-level mental health and psychosocial support (MHPSS) interventions.
Activities include:
- Funding studies to understand better the effectiveness and implementation of community-level MHPSS interventions.
- Supporting a cross-study learning collaborative to facilitate connections and coordination across study teams and between study teams and technical and policy partners at the local, national, regional, and global levels.
- Establishing an implementation science collaborative network on MHPSS, which is connected to existing MHPSS communities of practice and networks.
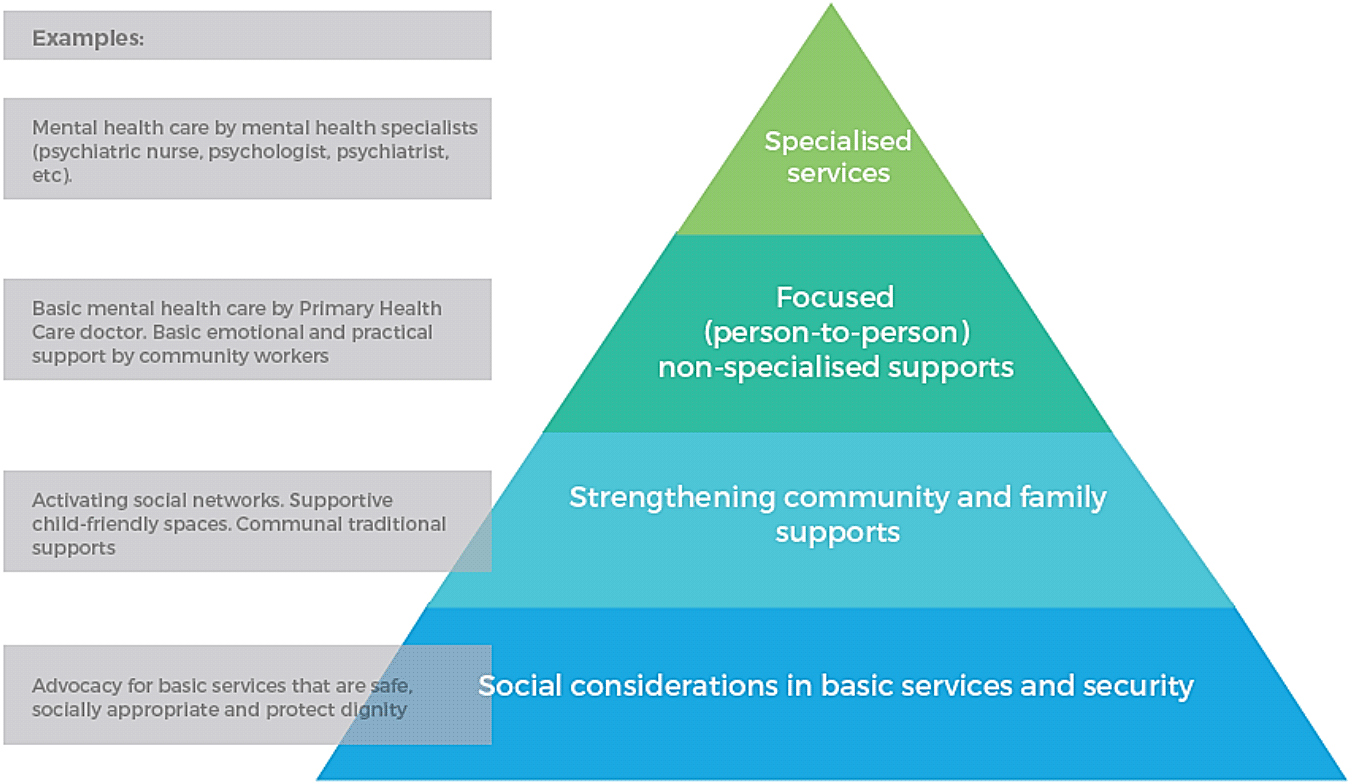
IASC Levels of MHPSS Intervention
One of the biggest challenges facing survivors of torture and those living in emergency contexts is the lack of mental health care and psychosocial support. Mental health and psychosocial support interventions (MHPSS) are defined as “any type of local or outside support that aims to protect or promote psychosocial wellbeing and/or prevent or treat mental disorders.” (IASC, 2017) MHPSS interventions are commonly used by non-governmental and humanitarian organizations in challenging settings to improve psychosocial wellbeing and mental health. In many settings however, trauma-exposed individuals enter the mental health system through general community- or primary care level services, rather than through interventions explicitly targeting Victims of Torture or other trauma exposed individuals. Therefore, improving access to these services broadly will directly benefit survivors or torture and traumatic events related to war.
Partnerships
Activities
There are four studies which seek to better understand the effectiveness and implementation of community-level Mental Health and Psychosocial Support (MHPSS) interventions, with an emphasis on the PSS intervention components and impacts.
A fifth, related study is being funded by GIZ and will be implemented by War Child in Jordan. This collection of studies spans seven countries in four regions—South Asia, the Middle East, Central and South America, and Africa.
To learn more about these interventions, visit the Mental Health and Psychosocial Support Knowledge Hub.
Resources
Hosted by the Center for Innovation in Mental Health (CIMH) at the CUNY SPH, the Mental Health and Psychosocial Support (MHPSS) Knowledge Hub provides an in-depth overview of the topic area and specific interventions.
The following resources and reports provide additional information on the frameworks and programs utilized by study partners (click to download):
Identifying research priorities for psychosocial support programs in humanitarian settings